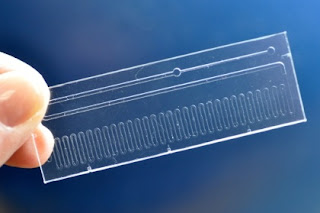
The sleek contraption that won this year’s UK Design Award doesn’t resemble a living organ. But this translucent, glowing microchip, with slender tubes branching off of it, breathes just like a human lung.
The device, which was created by researchers at Harvard’s Wyss Institute for Biologically Inspired Engineering, is made from a rubber-like polymer and is a mixture of biological human cells and fluid that mimics blood.
The lung device is just one of several “human organ simulators” designed by the researchers, Daniel Huh, a former Wyss Institute Fellow and assistant professor in bioengineering at the University of Pennsylvania, told me over the phone. “They are tiny microchips about the size of a computer memory stick that we use to grow living cells, and mimic the most important structure and function of human organs.”
Huh and his colleagues have already made devices that mimic lungs, kidneys, and skin.
“We’re doing many different organs and by having a common blood vessel channel, we can actually link them together to eventually create a human body on a chip,”Donald E. Ingber, bioengineer and Wyss’ Founding Director, told me. “We’ve already connected four different organ on chips together and kept them alive on an automated instrument for two weeks.”
The researchers aim to use the devices to create a more holistic representation of the human body, making drug testing models cheaper, more ethical, and more effective. “It would allow us to mimic the human biology and physiology at the whole body level, not just at the individual level,” said Huh.
“Our design was motivated by one of the most critical medical challenges that we’re facing: That the animal models that we use for developing and testing new drugs are for the most part failing to predict how humans respond to drugs,” he said. “The biology of animals like mice is completely different than that of humans.”
The lung on a chip was made using a microfabrication process adapted from the computer chip industry. It sandwiches two layers of living tissue composed of cells from the lung’s air sacs and the surrounding blood vessels across a porous rubber membrane containing hollow microchannels. A culture medium mimicking blood flows in the capillary channel, and a regular mechanical stretching function mimics breathing motions. Air and fluid are delivered via tubing connected to the microchip by using a syringe and vacuum pumps.
What’s exciting about the device is its ability to replicate complex biological processes. For example, when bacteria is placed on the surface of the chip to mimic a lung infection, and white blood cells taken from the human body are placed into the blood capillary channels of these devices, the chip reacts fiercely.
“The white blood cells circulating in the capillary channel stick to capillary cells, get across the tissue layer, show up on the lung surface and start engulfing the bacteria,” said Huh. “Just as they would do in a lung in the human body.”
Currently, drug developers either test drugs on animals or use a cell culture model where they take living cells from a human body, grow them in a petri dish, then test drugs on them. While animal testing evokes ethical issues, the petri dish approach hardly replicates all the complexities of the human body with its beating heart, contracting muscles, and constant blood flow.
“If you think about it, this is such an unnatural, uncomfortable environment for these cells. They are used to very complex, dynamic three-dimensional environments in the human body,” said Huh.
He explained that traditional drug testing methods are largely failing to predict the effects of drugs at a preclinical stage. This has a knock-on effect at the human trial stage as both time and money are ill-spent on drugs that end up having no impact.
“The idea here is by developing next-generation drug testing technologies we can use the preclinical stage to weed out the drugs that are destined to fail as early in the process as possible,” said Huh. This, he explained, would dramatically reduce both the cost and time required to develop effective drugs in the future.
The lung on a chip was made using a microfabrication process adapted from the computer chip industry. It sandwiches two layers of living tissue composed of cells from the lung’s air sacs and the surrounding blood vessels across a porous rubber membrane containing hollow microchannels. A culture medium mimicking blood flows in the capillary channel, and a regular mechanical stretching function mimics breathing motions. Air and fluid are delivered via tubing connected to the microchip by using a syringe and vacuum pumps.
What’s exciting about the device is its ability to replicate complex biological processes. For example, when bacteria is placed on the surface of the chip to mimic a lung infection, and white blood cells taken from the human body are placed into the blood capillary channels of these devices, the chip reacts fiercely.
“The white blood cells circulating in the capillary channel stick to capillary cells, get across the tissue layer, show up on the lung surface and start engulfing the bacteria,” said Huh. “Just as they would do in a lung in the human body.”
Currently, drug developers either test drugs on animals or use a cell culture model where they take living cells from a human body, grow them in a petri dish, then test drugs on them. While animal testing evokes ethical issues, the petri dish approach hardly replicates all the complexities of the human body with its beating heart, contracting muscles, and constant blood flow.
“If you think about it, this is such an unnatural, uncomfortable environment for these cells. They are used to very complex, dynamic three-dimensional environments in the human body,” said Huh.
He explained that traditional drug testing methods are largely failing to predict the effects of drugs at a preclinical stage. This has a knock-on effect at the human trial stage as both time and money are ill-spent on drugs that end up having no impact.
“The idea here is by developing next-generation drug testing technologies we can use the preclinical stage to weed out the drugs that are destined to fail as early in the process as possible,” said Huh. This, he explained, would dramatically reduce both the cost and time required to develop effective drugs in the future.
0
comments